Reevaluating Obesity: The Shift from BMI to a Comprehensive Health Assessment
Recent developments in the field of health and obesity research have highlighted the limitations of the traditional Body Mass Index (BMI) as a gauge for assessing weight-related health risks. With over 100 million Americans classified as overweight, new standards propose that many of these individuals may actually fall into the obese category. This shift calls for a more nuanced understanding of obesity that includes not just weight, but also waist-to-hip ratios and various health markers.
Limitations of BMI
BMI has long been the standard tool for determining whether an individual is underweight, normal weight, overweight, or obese, calculated using height and weight. However, experts from the European Association for the Study of Obesity (EASO) argue that this metric often underestimates the health risks associated with obesity. Relying solely on BMI can obscure critical information about fat distribution in the body, potentially leading to misdiagnosis and inadequate health interventions.
According to recent findings, a significant number of individuals previously classified as “overweight” based on BMI may actually meet the criteria for obesity when considering factors such as waist circumference and metabolic health indicators like liver enzymes and insulin levels. A study conducted by researchers at the American College of Physicians revealed that nearly 19% of adults previously labeled as overweight were reclassified as having obesity under the new European standards. If these criteria were applied to the broader American population, approximately 20.7 million people could be misidentified as merely overweight.
The Health Implications of Misclassification
This reclassification carries substantial health implications. The EASO framework emphasizes the importance of assessing obesity risk beyond BMI, especially as healthcare providers increasingly consider the effectiveness and costs of weight-loss medications. The traditional reliance on BMI has left healthcare providers inadequately equipped to evaluate the complexities of individual health profiles.
Amy Woodman, a registered dietitian, notes that BMI is just one piece of a larger puzzle. She emphasizes the need to consider a patient’s dietary habits, physical activity levels, and any coexisting health conditions to provide a comprehensive assessment of their health status.
Understanding Fat Distribution
Crucial to understanding obesity is the distribution of body fat. For example, a high waist-to-hip ratio indicates a higher concentration of visceral fat around the abdominal area, which is linked to a greater risk of serious health issues like heart disease and diabetes. Conversely, a lower waist-to-hip ratio, typical of a “pear-shaped” body, suggests that fat is distributed more around the hips and thighs, which poses less of a health threat.
Dr. Britta Reierson, an obesity medicine specialist, points out that a holistic assessment of health must include not only weight but also factors like muscle mass, existing health conditions, and metabolic markers. This comprehensive approach allows healthcare providers to better understand their patients’ health risks.
Prevalence of Obesity and Associated Health Risks
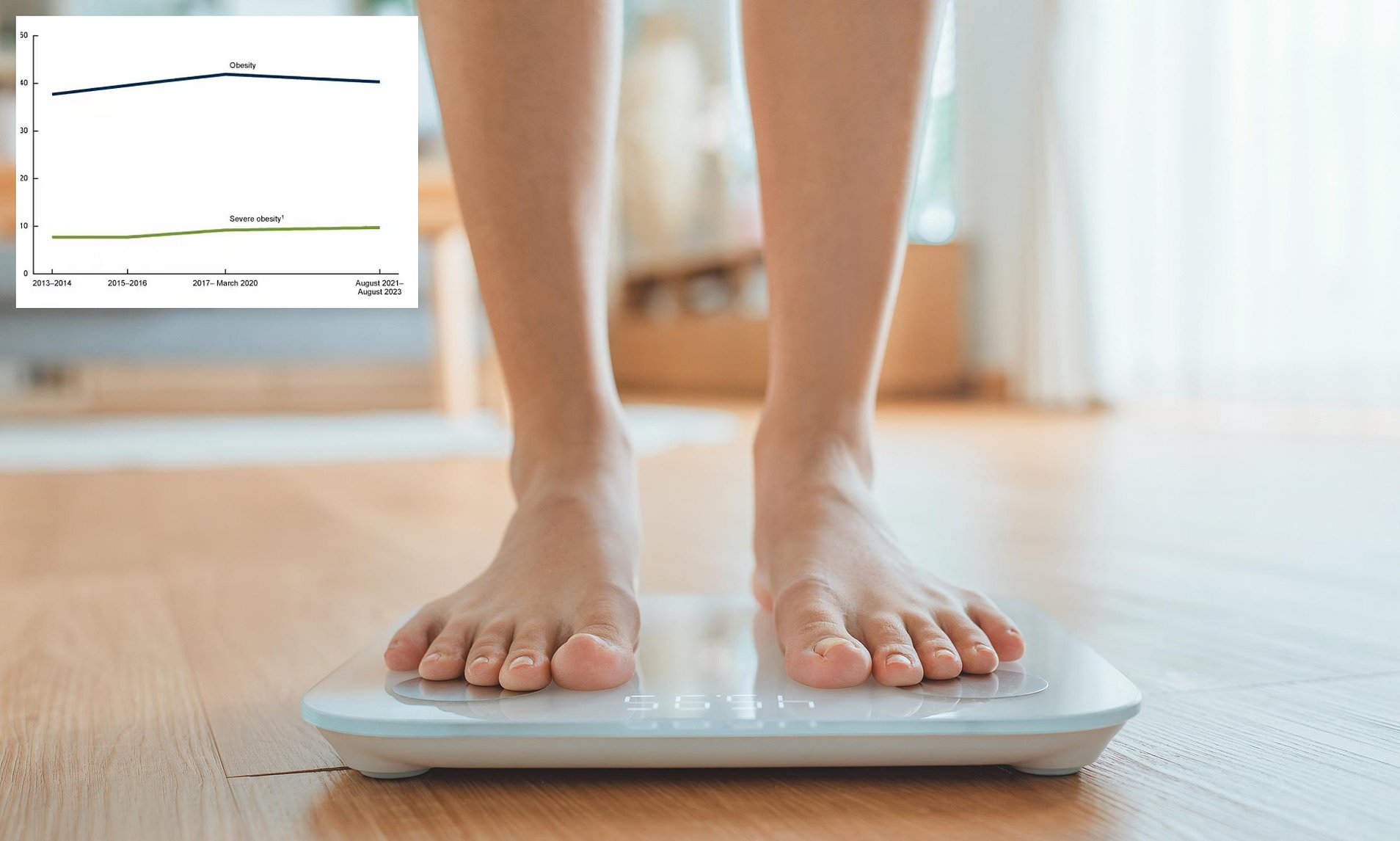
The recent reclassification of individuals has revealed troubling statistics regarding obesity in America. Approximately 40% of the American population is now considered obese, showing a slight decrease from previous years, yet still indicating a persistent public health crisis. Among those newly classified as obese, the most common health issues included high blood pressure, arthritis, and diabetes.
Interestingly, while individuals classified as overweight by the new standards had a 46% lower risk of death compared to those with normal weight, the newly identified obese individuals did not have a significantly higher mortality risk compared to the general normal-weight population. However, when compared to healthy individuals without any underlying health conditions, the risk of death was indeed elevated among those newly classified as obese.
A Broader Perspective on Health Indicators
As the medical community grapples with these findings, there is a growing consensus that BMI should not be the sole measure of health. Dr. Michael Aziz, an internal medicine physician, reiterates that waist-to-hip ratio is a more accurate indicator of health risks. This perspective is echoed by a global panel of experts who have called for a more comprehensive approach to assessing health that goes beyond BMI.
The transition to these new standards marks a significant step forward in highlighting the importance of evaluating a range of health metrics. Dr. Reierson advocates for wider acceptance of these standards in clinical settings, emphasizing that while BMI can provide insights into metabolic health, it should not dictate the entirety of a patient’s health assessment.
Conclusion
The evolving debate around obesity and health assessment underscores the need for a more multifaceted approach to understanding weight and its associated risks. As healthcare providers begin to adopt a broader range of metrics, the goal is to foster a more accurate understanding of individual health, ultimately leading to better outcomes for patients. The move away from sole reliance on BMI is not just a trend; it reflects a deeper understanding of the complexities of health and obesity in modern society.